Echocardiography is a non-invasive test, which through the use of ultrasound in a frequency range of 2 to 10 MHz allows us to explore the anatomy and function of the heart. The exam consists of several phases (one-dimensional, two-dimensional, three-dimensional, doppler and colordoppler analysis) which together provide complete information allowing to perform detailed measurements and analysis of cardiac structures. With improvement in technology, echocardiography has progressively replaced other more invasive tests that were previously necessary to diagnose some heart diseases. It can be performed at the patient’s bedside and allows you to get information directly during the examination (Figure 6).
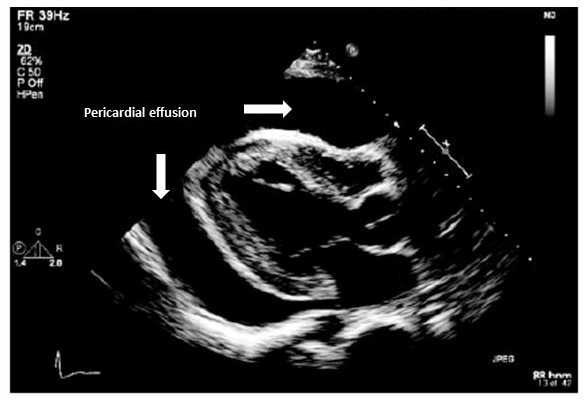
Figure 6. Presence of hemodynamically significant pericardial effusion in the 4th post-operative day in a patient undergoing surgical myocardial revascularization.
There are no risks for the patient undergoing an echocardiographic examination (since it is an ultrasound technique, it is based, unlike X-rays, on the use of acoustic and non-electromagnetic waves), however its reliability depends very much on skill and operator experience. Furthermore, in some patients with lung diseases or in obesity it may be difficult to obtain quality images due to the inability of ultrasound to penetrate adequately into the chest.
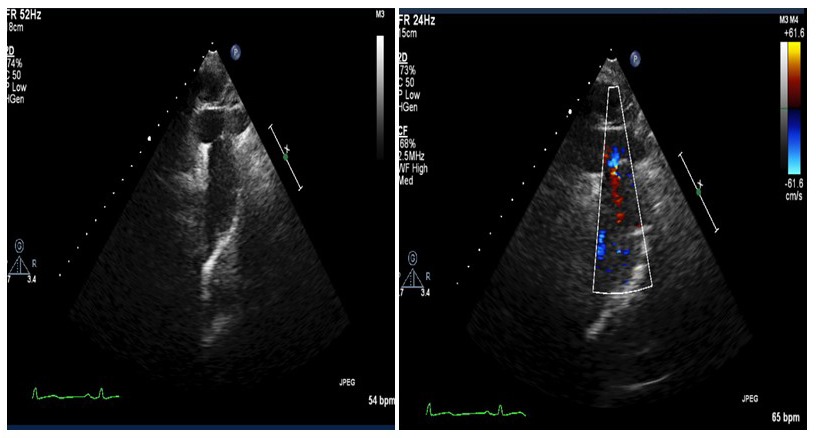
Figure 1. The echocardiography analysis of the aortic arch reveals the presence of severe aortic coarctation in a 48-year-old man with a history of arterial hypertension resistant to multi-drug therapy.
Echocardiography thanks to its versatility can be applied in various clinical scenarios:
- On an outpatient basis as a screening test in a patient with a suspected heart disease, Figure 1 and 2; or in the follow-up of patients with known heart disease;
- In cases of Urgency-Emergency to confirm a life-threatening diagnosis (eg cardiac tamponade);
- In the cardiac surgery operating room, through a transesophageal method, to guide the surgical procedure (for example in the valve repair) and to give “live” information on the success of surgery;
- In coronary and post-surgical intensive care as a monitoring tool for cardiac function, capable of guiding weaning from life support therapies and/or diagnosing acute complications of myocardial infarction in time;
- In the cath lab as a guide to the percutaneous treatment of cardiac pathologies (eg closure of atrial septal defects, mitral valve repair, left atrial occlusion, etc.)
In the hands of medical personnel specifically trained in “cardiovascular imaging” using the latest equipment, the basal and advanced echocardiographic diagnostics appears an essential tool in all patients with known or suspected heart disease.
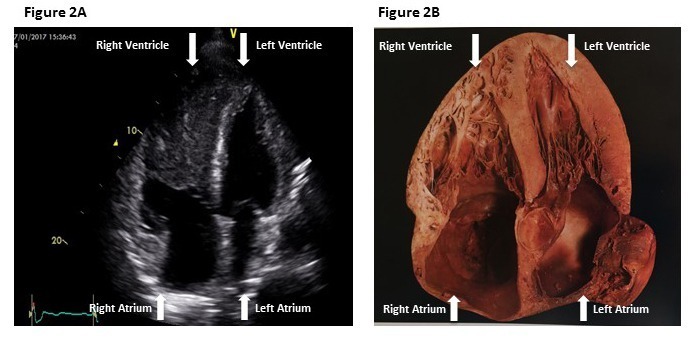
Figure 2A. Apical approach with visualization of the 4 cardiac chambers; mass evidence within of the right ventricle (metastasis of renal rabdiomyosarcoma) in a patient in the cardiology department for signs of heart failure.
Figure 2B represents the longitudinal section of a healthy heart (image turned upside down to make it comparable with the ultrasound visualization of figure 2A) and allows to appreciate the high diagnostic sensitivity of the echocardiographic method in the study of cardiac anatomy.
It is essential to bear in mind that a good echocardiographic evaluation always follows a detailed clinical and anamnestic analysis of the patient. There are several diagnostic echocardiographic methods, as described below, each of which cannot disregard the correct indication to the exam.
Echocardiography and transthoracic echocolor Doppler: performed using a transthoracic approach (the echocardiographic probe is placed on the patient’s chest), studies in detail the morphology and mechanical function of the heart as pump, of the proper function of the valve apparatus. It is capable of identifying congenital and/or acquired pathological changes and assessing how much the pathological element (eg a valve defect) impairs global cardiac function and its anatomy. The combination of this information and the clinical data guides the therapeutic choice both in terms of medical versus surgical therapy and the type of surgical technique to be used; figure 5.
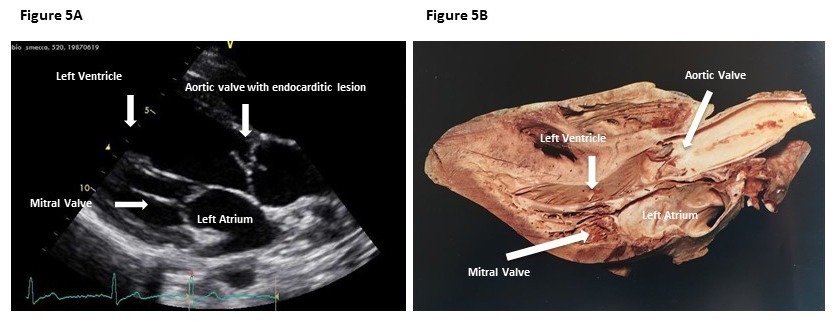
Figure 5A. Left parasternal long axis projection: evidence of endocarditic lesion on bicuspid aorta valve at high embologenic potential in a young patient with persistent fever.
Figure 5B represents the longitudinal section at the level of the left outflow tract of a heart.
Transesophageal echocardiography: performed through the use of an echocardiographic probe inserted through the first part of the digestive canal (esophagus) allows, thanks to the anatomical proximity between the esophagus and the heart, a posterior visualization of the cardiac structures with higher resolution and diagnostic specificity. It is a decisive examination in the solution of some diagnostic questions. This can happen due to the presence of a poor quality transthoracic acoustic window (for example in emphysematous patients) or in the presence of artificial metal structures (mechanical valve prostheses) that create reverberations and image artifacts. To exclude the presence of thrombi and endocarditic lesions (infections of the heart). To study in detail the cardiac anatomy for a reparative treatment (eg closure of an atrial septal defect, mitral repair).
Pharmacological stress echocardiography: involves the administration of a pharmacological stimulus (stress) and allows to study the behavior of the cardiac muscle or the changes in the valvular hemodynamic parameters during the increase in workload. The pharmacological echostress serves to define the nature of the patient’s symptoms, to ascertain the functionality of the cardiovascular system and to decide, based on the outcome, a further clinical and therapeutic procedure.
Contrast echocardiography: It involves the intravenous administration of a contrast agent while performing a transesophageal or transthoracic echocardiogram. The contrast agests used in echocardiography are different from the traditional radiological contrast ones. The echocontrastographic effect is due to the formation of microbubbles which, by increasing the reflection of the ultrasounds, enhance the acoustic signal and improve the quality of the echocardiographic image (better definition of the endocardial edges and valve flows, possibility of evaluating coronary perfusion). It is possible to exclude the presence of thrombus and/or make a diagnosis of non-compacted myocardium.
Bubble contrast Echocardiography with an injection into a vein of a sterile salt solution shaken into microbubbles or “bubble test” recommended for the diagnosis of congenital heart disease with right-to-left shunt and/or suspected embolic heart disease (patent foramen ovale, PFO), (Figure 3).
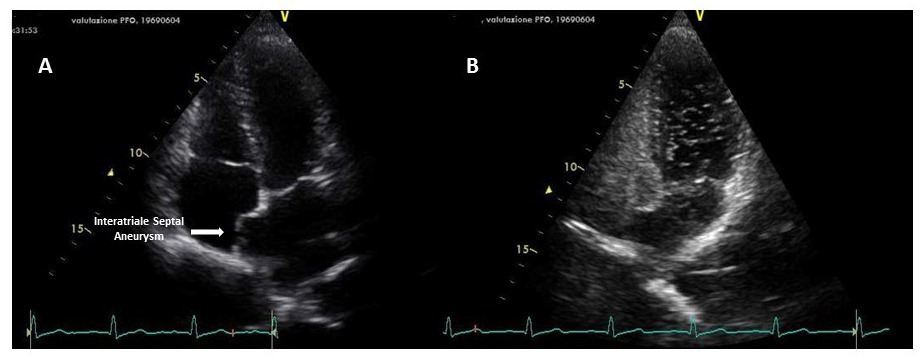
Figure 3. Evidence of interatrial septal aneurysm (figure A) with microbubble passage from right to left during Valsalva maneuver. (Figure B) in a patient with recurrent episodes of cerebral ischemia. Diagnostic examination for patency of the oval foramen.
Three-dimensional echocardiography in real time (3D-RT) is a complementary and non-alternative method to the two-dimensional one, with the advantage of representing the individual components of cardiac structures (eg the valve apparatus or the interatrial septum) in their complex 3D structure and in their mutual spatial relations. 3D-RT echocardiography is mainly used in the study and treatment of valvular diseases. It allows to identify the mechanism of mitral regurgitation and identify the culprit lesion. It is the non-invasive method of reference in the evaluation of the anatomical valve area of mitral stenosis and represents an indispensable guide in the percutaneous treatment of valvulopathies. (Figure 4)
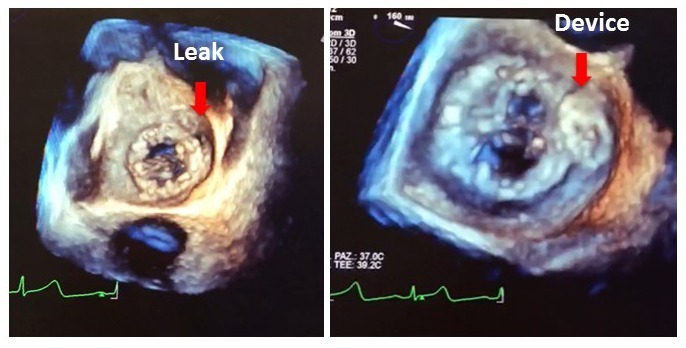
Figure 4. Pre and post 3D echocardiography (left and right image respectively) percutaneous closure of mitral paraprosthetic leak.
Fetal echocardiography: performed by transabdominal approach (the echocardiographic probe is placed on the mother’s abdomen), and used in the second trimester of pregnancy as a screening procedure for the early diagnosis of congenital heart disease in the fetus. The incidence of congenital heart disease is around 8-10/1000 live births. With the improvement of technology it is possible to diagnose most of the congenital heart defects before birth. The counseling (informational interview) of congenital heart disease in the fetal age is an integral part of the exam and the gynecologist and pediatric cardiologist must always be involved. In fact, a diagnosis of complex congenital heart disease associated with other malformations that compromise the survival of the fetus, if it occurs before the 23rd week of gestation, may lead to the decision to voluntarily terminate the pregnancy.
© Margherita Ministeri for salvatoretribastone.com © ALL RIGHTS RESERVED

