Coronary surgery is more than fifty years old. The first interventions of aortocoronary Bypass were carried out in 1964 and only at the end of the sixties we began to talk about new techniques and the use of the mammary artery. From the seventies to the present day the techniques have evolved more and more and despite the development of percutaneous treatment (angioplasty), even today, according to the international guidelines, surgery remains the ideal therapy for many coronary patients.
The purpose of the surgical treatment is to overcome the obstacle constituted by a critical narrowing (stenosis) in one of the coronary arteries through a bridge (bypass) that restores the blood flow over the obstacle, thus favoring the supply of oxygenated blood to the myocardial cells of the coronary area.
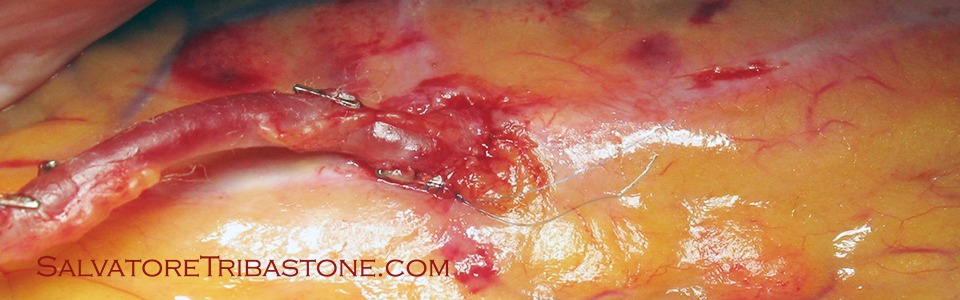
To do this, a conduit is required that must be positioned beyond the stenosis. The internal mammary artery (IMA) is the ideal conduit that is normally used on the main coronary branch, the anterior descending artery. For the other coronaries, conduits such as the great saphenous vein (GSV) taken from the patient’s leg are used, and less frequently, the radial artery and the gastroepiploic artery. The number of bypasses depends on the number of blocked arteries. The vast majority of cardiac surgery centers use bypass in mammary artery and saphenous vein. It is possible to use the double mammary (right and left) for a complete revascularization with totally arterial conduits.
The revascularization with a mammary artery (the left is the most used for anatomical proximity with the anterior descending artery) offers the best results in the long term. It is taken from the internal thoracic wall after the opening of the thorax by sternotomy. The mammary artery is isolated and detached from the thorax by binding the collaterals and the terminal part is sutured (anastomosis) downstream of the stenotic coronary artery. The saphenous vein, isolated from the patient’s leg, is sutured downstream of the coronary stenosis and on the ascending aorta from which it will receive the blood for the coronary artery after the stenosis as seen from the figure (in blue the vein graft which constitutes the aorto-coronary bypass and in red the peduncle of the mammary artery on the coronary).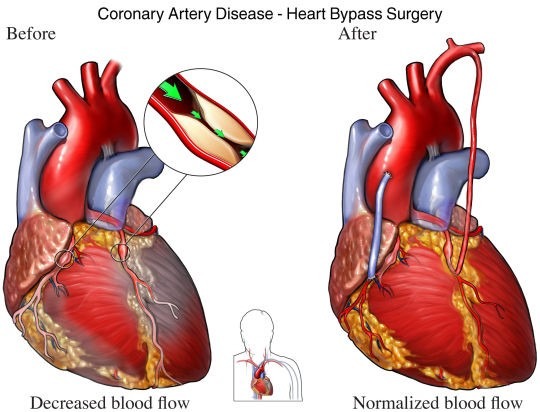
The operation can be performed in cardiopulmonary bypass (CPB) with a fixed heart, or without the aid of CPB, with a beating heart (off-pump), a decision that is done according to the patient’s general conditions when the CPB could increase the risk of postoperative complications of organs such as the kidney, the brain, the lung and the heart itself. Another solution could be the one of the hybrid approach that involves traditional surgery and angioplasty (percutaneous treatment) to complete the revascularization of non-surgical vessels. Furthermore, the treatment of the anterior descending artery with mammary artery in a beating heart followed by the percutaneous procedure on the other vessels can be extremely beneficial for high risk patients who would not tolerate an extracorporeal circulation.
The role of the Heart Team (usually heart surgeon, cardiologist and anesthesiologist) is to carefully evaluate the risks of surgery in complex patients with multi-organ pathologies. The multispecialist approach, with the advice of the neurologist, nephrologist, hematologist, pulmonologist and others, improves the preoperative assessment of the critical patient through strategies that tend to reduce the impact of complications during surgery and immediately after surgery.
The use of scores, of which the most used in the world are Euroscore II and STS Score, greatly helps in identifying high-risk subjects that could be referred to other therapeutic solutions rather than surgery.
The benefits of myocardial revascularization by coronary artery bypass grafting:
- increased flow of blood, oxygen and nutrients for myocardial cells;
- reduction or disappearance of pain (angina) typical of coronary heart disease;
- reduction of adverse events in the short and long term if combined with a careful monitoring of risk factors;
- improvement of the quality of life.
Like all surgical procedures, myocardial revascularization is not free of complications, sometimes very serious, that can lead to death. Fortunately, serious complications are not frequent and depend mainly on pre-existing diseases. Among the major and minor complications we can list:
- perioperative myocardial infarction;
- arrhythmias;
- cerebral stroke or transient cerebral ischemic attack;
- postoperative bleeding;
- kidney failure;
- perioperative infection;
- congestive heart failure;
- hematological complications;
- pulmonary complications.
The patient who has undergone a bypass resumes normal life after a few days of rehabilitation (recommended!).
We should also remember that the bypass surgery is still a ‘palliative’ that does not remove the causes of atherosclerosis that damaged the coronary arteries. Only the careful reduction of risk factors can improve the ‘quoad vitam’ outcome and prevent further injuries from recurring in the future, invalidating the good work done by the cardiac surgeon.
© ALL RIGHTS RESERVED